- Visibility 160 Views
- Downloads 47 Downloads
- DOI 10.18231/j.adr.2024.024
-
CrossMark
- Citation
Surgical management of neurofibroma of gingiva with diode laser: A case report
Introduction
Neurofibroma is considered as a benign neoplasm of peripheral nerve sheath which is characterized by the Schwann cell proliferation, proliferation of perineural cells and endoneural fibroblasts.[1] It can be classified into solitary or multiple neurofibroma depending on their involvement, a majority of solitary neurofirbroma are sporadic whereas the minority of it are associated with neurofibromatosis type -1.[2] Solitary neurofibroma has an unknown etiology. Moreover, as evidenced by the literature 6.5%[3] of solitary neuofibromas remains unassociated with type -1 neurofibromatosis.Oral neurofibroma is usually a small, well circumscribed, but not encapsulated, tumor. Histopathologically, Areas of myxoid and/or hyalinized changes are common in this type of tumours.[4], [5], [6], [7]
It has a loosely textured growth with irregularly arranged nerve fibres divided by elongated cells and collagen fibrils unevenly distributed. There are poorly developed mutinous stroma and areas containing spindle cells. Although oedematous change is more likely especially in the plexiform variety, frequently mast cells are present with scanty reticular fibres randomly deposited, and in older lesions hyaline changes may occur. The plexiform neurofibroma can clearly be demarcated from the other neurofibromata on the basis of pathology and it presents a problem of classification. It occurs either as a solitary lesion or with other manifestations of neurofibromatosis but Harkin and Reed (1968) states, that all reports of solitary lesions have neurofibromatosis, is now a controversy as more cases of solitary plexiform neurofibroma are detailed.
The current treatment of neurofibroma is complete resection. These tumors are non-radiosensitive and limited benefit had been observed with chemotherapy. The recurrence is seen in as many as 20% of the patients with a neurofibroma after complete resection and increases to 44% with subtotal resection.[8]
To add on, differential diagnosis of swellings of intraoral origin includes fibroma, schwannoma, hemangioma, and lipoma.[2] Here we report a rare case of solitary neurofibroma of gingiva in the mandibular anterior region and was excised using diode laser.
Case presentation
A female patient, 33 years old, was presented to the private dental clinic with a chief complaint of localised painless gingival swelling in her lower front tooth region for 3 months. Further, the patient gave a past history of similar growth which was surgically excised in the same tooth region 2 years back. The medical history was non‑contributory. Intraoral examination revealed a non-ulcerated, sessile, diffuse growth involving the marginal and attached gingiva corresponding to teeth #31 ([Figure 1]).



|
Author &year |
Location |
Clinical and histological presentation presentation |
Managment |
Recurrence |
|
Suramya S,2013 [9] |
Maxillary anterior gingiva |
Pedunculated, bilobulated growth was located on the marginal ridge extended palatally. Histopathologically, superficial stratified squamous parakeratinized epithelium. Connective tissue showed presence of tumour mass consisiting of cells arranged in fascicles |
Surgical excision |
No recurrence after 12 months |
|
Babita Pawar, 2013 [10] |
right maxillary gingiva |
firm with sessile base, smooth, non- painless, ulcerated, with normal color measuring 4 mm × 10 mm, extending from the mesial of maxillary right first premolar to the mesial of maxillary right first molar involving the marginal, papillary, and attached gingiva, Histopathologically, spindle-shaped cells, with fusiform or wavy comma-shaped nuclei distributed on a background of delicate connective tissue matrix |
Surgical excision |
No recurrence after 12 months |
|
Joann Pauline George, 2015 [11] |
lingual gingiva of the mandibular posterior region |
Elliptical gingival overgrowth (GO), solitary, pink, an erythematous patch on its dorsal aspect, smooth and regular margins. Histopathologically, hyperplastic, discontinuous and nonkeratinized stratified squamous epithelium with intercellular edema. Areas of ulceration covered with fibrinopurulent membrane, lesional cells arranged in the form of interlacing fascicles. |
Surgical excision |
No recurrence after 15 months |
|
Fabrício Rezende Amaral, 2018 [12] |
dorsal surface of the tongue |
Two nodules with a firm consistency and color similar to mucosa located on the dorsal surface of the tongue, Separation of anterior teeth, alveolar bone expansion and overgrowth of attached gingiva without inflammation were observed. Histopathologically, Connective tissue with fusiform cell proliferation. Cells had basophilic and wavy nuclei and scanty cytoplasm permeated by collagen fibers and nerve bundles. |
Excision with diode laser |
-- |
|
Mohammed M. Al-Ali, 2024 [13] |
Maxillary anterior |
painless, solitary, oval, bi-lobulated, firm, pink, pedunculated and exophytic soft tissue mass on the upper right anterior alveolar ridge, in the area of the incisors, extending to the mesial surface of the canine and measuring 1.2×1.7 cm, Histopathologically, submucosal lesion arranged in a multinodular and plexiform pattern. The nodules were composed of haphazardly arranged spindle cells, one with elongated buckled and wavy nuclei (Schwann cells) and rest with ovoid nuclei (fibroblast) with spread apart collagen fibers having variable thickness all over the nodule in myxo-collagenous stroma surrounded by a fibrovascular connective tissue |
Excision with diode laser |
No recurrence after 36 months |
|
Our case |
Mandibular anterior |
Swelling was firm and painless and measured around 10mm in diameter, polpyoid lesion covered by stratified squamous mucosa. Focal ulceration and polymorphonuclear infiltration is noted in the epithelium and the underlying stroma. The stroma is composed of diffusely arranged bland spindle cells with wavy nuclei and fragments of collagen against a myxoid background. |
Excision with diode laser |
No recurrence after 3 months |
On palpation the swelling was firm and painless and measured around 10mm in diameter. The patient’s oral hygiene maintenance was unsatisfactory. The patient had unsatisfactory oral hygiene maintenance. No similar growth was noted on any other part of the body.
The differential diagnosis of fibroma was made based on the texture of the gingival growth. An excisional biopsy using a diode laser followed by histopathological examination was planned.
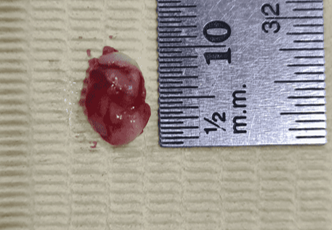
The lesion was excised using a diode laser of 810nm with 1W power setting under local anesthesia. The excised mass was almost 10mm in diameter ([Figure 2]).
It was then stored in 10% formalin and sent to histopathological evaluation. The patient was followed up for upto 6 months and showed no signs of recurrence ([Figure 3], [Figure 4]).
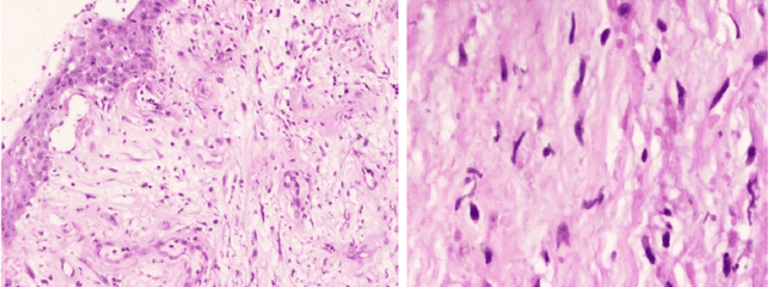
Histopathological findings ([Figure 5]): On histopathological examination the hematoxylin and eosin stained sections showed a polpyoid lesion covered by stratified squamous mucosa. Focal ulceration and polymorphonuclear infiltration is noted in the epithelium and the underlying stroma. The stroma is composed of diffusely arranged bland spindle cells with wavy nuclei and fragments of collagen against a myxoid background.
Based on the above clinical and histopathological findings, the diagnosis of neurofibroma was made.
Discussion
Oral neurofibroma is an uncommon benign tumor of nerve cell origin. They are often present as a part of neurofibromatosis–I or as an uncommon solitary condition. As per the literature, solitary neurofibroma is a benign, relatively circumscribed, slowly growing lesion which is not commonly associated with hereditary factors as in case of disseminated form.[14] Controversial facts are presented related to the cells of origin for neurofibroma. Based on the evidence, it may develop from the perineural fibroblast or the Schwann cell. Perineural fibroblasts are neuroectodermal tissue cells that are associated with the production of collagen which forms a network that encircles the individual axis cylinders of the nerve fibers alongside their associated Schwann cells. The etiology of solitary neurofibroma is still unknown. About 50% of cases are reported to be the result of spontaneous mutation. Common locations of the oral solitary neurofibromas include tongue (26%), buccal mucosa (8%), alveolar ridge (2%), labial mucosa (8%), palate (8%), gingiva (2%) as well as paranasal sinuses, floor of the mouth, nasopharynx, larynx and salivary glands. The lack of major nerve trunks in gingiva makes it a rare site of occurrence of solitary neurofibromas as in the present case.
In the oral cavity, neurofibromas range from a few millimetres to several centimeters and typically present as non‑tender, uninflamed, discrete mass. There is no gender or racial predilection. [15] Usually patients are asymptomatic, nevertheless, depending on the location (eg: tongue, palate) there are chances of getting traumatized that can give rise to associated symptoms. In the present case, the lesion was painless and the patient noticed it by herself.
The treatment modalities for solitary oral neurofibromas depend on the extent and the site of the lesion and it includes surgical excision using conventional scalpel, electrocautery and the laser excision. In this case, the lesion was close to 10mm in diameter, the laser excision was preferred to reduce the risk of bleeding. The beneficial property of diode laser (being the relatively easier method for soft tissue ablation with additional hemostatic and bactericidal effects) resulted in better results. [16]
Usually, solitary neurofibroma has an extremely good prognosis, with only rare reporting of recurrence after resection. Hence, this present case was kept under observation and was followed up every 3 months up to 6 months and developed no signs of recurrence.([Table 1]).
Conclusion
Solitary neurofibroma of gingiva is a rare oral lesion. Hence, it must be considered as a differential diagnosis of other swellings of intraoral origin and intraosseous lesions of the jaws. These lesions have a potential for malignant transformation, although these are benign tumors and have reported to have a fairly good prognosis. Therefore, these lesions must be evaluated and monitored carefully following a meticulous treatment plan. Novel surgical approaches can help in minimizing surgical trauma and thus improving the quality of life in such patients.
Source of Funding
None.
Conflict of Interest
None.
References
- J Holt. Neurofibromatosis in children. . AJR 1978. [Google Scholar]
- D Richards. Neurofibro Neurofibroma of the oral cavity.. Brit J Oral Surg 1983. [Google Scholar]
- MS Campos. Clinicopathologic and immunohistochemical features of oral neurofibroma. . Acta Odontologica Scandinavica 2012. [Google Scholar]
- HM Cherrick, LR Eversole. Benign neural sheath neoplasm of the oral cavity. Oral Med Oral Pathol 1971. [Google Scholar]
- SY Chen, AS Miller. Neurofibroma and schwannoma of the oral cavity. A clinical and ultrastructural study. Oral Surg. Oral Med Oral Pathol 1979. [Google Scholar]
- BA Wright, D Jackson. Neural tumors of the oral cavity. A review of the spectrum of benign and malignant oral tumors of the oral cavity and jaws. Oral Surg. Oral Med Oral Pathol 1980. [Google Scholar]
- E Chrysomali, SI Papanicolaou, NP Dekker, JA Regezi. Benign neural tumors of the oral cavity. A comparative immunohistochemical study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol Endod 1997. [Google Scholar]
- TS Bharath, YR Krishna, GR Nalabolu, S Pasupuleti, S Surapaneni, SB Ganta. Neurofibroma of the palate. Case Rep Dent 2014. [Google Scholar]
- Al-Ali Mm Al-Otaibi, L M, Al-Bakr, I. Excision of solitary non-syndromic oral plexiform neurofibroma utilizing a diode laser: A case report. Cureus [Internet] 2024. [Google Scholar]
- SS Shashikumar, HSS Kumar. Solitary plexiform neurofibroma of the gingiva: unique presentation in the oral cavity. J Clin Diagn Res 2013. [Google Scholar]
- JP George, S Jyothsna. Solitary neurofibroma: a rare occurrence on gingiva. Gen Dent 2016. [Google Scholar]
- B Pawar, A Tejnani, NK Sodhi, G Pendyala. A silent tumor of the gingiva: An unusual case report and surgical management with 1 year follow-up. J Indian Soc Period 2013. [Google Scholar]
- FR Amaral, M Ferreira, L Costa, P De Oliveira, BM Soares, P Souza. Use of Surgical Laser for Excision of a Neurofibroma Associated With Neurofibromatosis Type-1. J Lasers Med Sci 2018. [Google Scholar]
- KS Cunha, EP Barboza, EP Dias, FM Oliveira. Neurofibromatosis type I with periodontal manifestation. A case report and literature review. Br Dent J 2004. [Google Scholar]
- B Sivapathasundharam, S Lavanya, RS Ahathya, R Saravanakumar. Solitary neurofibroma of the gingiva. J Oral Maxillofac Pathol 2004. [Google Scholar]
- F Angiero, F Ferrante, A Ottonello, A Maltagliati, R Crippa. Neurofibromas of the oral cavity: clinical aspects, treatment, and outcome. Photomed Laser Surg 2016. [Google Scholar]
