Introduction
The name mucocele is derived from the Latin word’s mucus and cocele, which imply cavity and cavity respectively. A mucus-filled cyst that can develop in the oral cavity, appendix, gall bladder, paranasal sinuses, or lacrimal sac is known as a mucocele.1 It is characterized by the accumulation of mucus within the small salivary glands, resulting in a benign cystic lesion.1 They are not genuine cysts per definition. The sixteenth most frequent salivary gland lesion in the oral cavity is mucocele.2 The prevalence is considerable, with 2.5 lesions per 1000 people.3 The two clinical forms are extravasation and retention. Extravasation occurs when fluid escapes into the surrounding soft tissues from injured salivary gland ducts and acini, which is particularly prevalent in small salivary glands. Retention is caused by a blockage of a salivary gland duct, which is frequent in major salivary gland ducts.4
Mucoceles appear as blue, soft, translucent cystic swellings that usually disappear on their own. The blue colour is caused by vascular congestion, cyanosis of the tissue above, and fluid buildup below. The colour of the lesion, however, may vary depending on its size, closeness to the surface, and the flexibility of the underlying tissue. When this mucocele is situated on the floor of the mouth, it resembles the underbelly of a frog and is hence referred to as a ranula.5
Mucoceles are often asymptomatic, although they can occasionally cause discomfort by interfering with speaking, chewing, or swallowing. Surgical excision, marsupialization, micromarsupialization, cryosurgery, laser vaporization, and laser excision are all treatment possibilities.2
This article describes a recurrence case report of mucocele on lower lip treated by surgical excision method using scalpel blade.
Case Report
Clinical examination
A 10-year-old girl presented to the Oral Medicine and Radiology department with the chief complaint of painless swelling on her lower lip for two weeks. Swelling began modest and progressively increased to its current proportions. There was no substantial medical history to speak about. A spherical, single, fluctuant swelling was noticed on the inner side of the lower lip near the left lateral incisor area during an intraoral examination. Swelling was 4-5 mm below the lower lip's vermilion border, measuring roughly 4 mm 3 mm 2.5 mm. The swelling was whitish red in colour. On examination of the lesion, it was soft in consistency, fluctuant, and palpable with no increase in temperature and oval in shape. No other oral anomalies were detected. Patient gives history of trauma while eating 1 month back. Also, patient gives history of increase in size while mastication and decrease in size after some time. Thus, the provisional diagnosis of Mucocele was given.Figure 1
Investigations
Routine haematological investigations, such as hemograms, bleeding, and clotting time, revealed that everything was within normal physiological parameters. Patient was also asked to get tested for COVID 19 due to current ongoing situation.
Differential diagnosis
Fibroma, lipoma soft tissue abscess, oral hemangioma, oral lymphangioma, and benign salivary gland tumour were among the possible diagnoses.
Fibromas range in consistency from mild to very stiff. They are the most frequent type of intraoral soft-tissue lesion, and they most typically develop on the lips. Lipomas are neoplasms composed of mature adipose tissue that are uncommon in the oral cavity but can develop on the lips. Cysts, mucoceles, abscesses, and hemangiomas fluctuate, but lipomas and small salivary gland tumours do not.
Mucoceles appear pathognomonic, and the following information is critical: the position of the lesions, the history of trauma, the rapid appearance, size variations, the bluish colour, and consistency. Based on the history and clinical examination, a provisional diagnosis of mucocele was made. Surgical scalpel excision with local anesthesia was planned.
Treatment
Phase I treatment included a complete scaling and root planing as well as oral hygiene training. The patient was shown the correct technique of brushing (Modified Bass Technique). A 0.2% mouth-rinsed chlorhexidine of 10 ml, 1:1, and twice daily for 15 days were recommended for patients.
Phase II therapy consisted of surgical excision of the lesion under local anesthesia. The patient was explained about the procedure and informed consent was obtained. The specimen was sent to a pathologist for histopathologic examination. Which confirmed the diagnosis of Mucocele. Analgesics, Antibiotics and post-operative instructions were provided. After one week, the patient was called back for suture removal, and wound healing was found to be satisfactory.Figure 2, Figure 3.
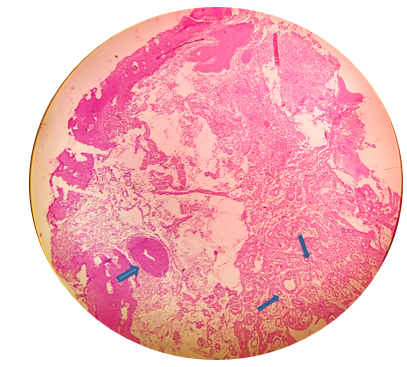
Patient reported to the department with the recurrence at the same sight after 15 days. Which was again incised thoroughly with underlying minor salivary gland. Patient was recalled after 7 days for suture removal. There was uneventful healing with some little scarring. Patient is since then on follow up and has not given complaint of recurrence since last 3 months. 4 magnification haematoxylin and eosin slice demonstrating mucin pooling areas in the middle luminal area surrounded by granulation tissue. The lesion's periphery exhibits salivary gland acini (indicated by arrow)Figure 4.
The overall histological findings were indicative of a mucous extravasation cyst, validating the mucocele diagnosis.
Discussion
Mucocele is a frequent oral mucosa lesion that can affect the entire population.6 The lower lip is thought to be the most often afflicted region (40 to 80 percent of all cases), followed by the cheek mucosa and the floor of the mouth.3 Although these lesions can arise at any age, children and young people are the most often afflicted. Both sexes are impacted equally.7 The two main etiological factors are:
The most prevalent cause of salivary secretion spilling into adjacent submucosal tissue is physical trauma. Inflammation may develop later as a result of the stagnated mucus. The habit of lip biting and tongue thrusting is one of the exacerbating factors. The extravasation type will evolve through three phases. Mucous will flow from the salivary duct into the surrounding tissue during the initial phase, showing some leucocytes and histiocytes. Due to the presence of histiocytes, macrophages, and large multinucleated cells associated with a foreign body reaction, granulomas will develop in the second phase, known as the resorption phase. Later in the third phase, connective cells will create a pseudo capsule surrounding the mucosa that is devoid of epithelium. As a result of duct dilation induced by a sialolith or thick mucosa, the retention form of mucocele is most often observed in the main salivary glands.4 Mucoceles can appear as a fluid-filled vesicle or blister in the surface mucosa, or as a fluctuant nodule deep inside the connective tissue. Fibrosis may be seen on the surface of long-standing lesions.8 The clinical characteristics and the history are pathognomic, leading to the diagnosis of mucocele. Mucocele histology typically reveals the presence of mucino phages in the collapsed wall of granulation tissue, as well as the development of a well-circumscribed, cyst-like area surrounded by granulation tissue.9
The primary goal of mucocele therapy is to completely eradicate the lesion to avoid recurrence. To avoid recurrence, we must eliminate the afflicted and neighbouring glands, as well as the diseased tissue. As therapies for mucocele, cryosurgery, micro marsupialization, marsupialization, surgical excision, and laser ablation have all been recommended.3
The surgical technique is the traditional way of therapy. It does not require specialised equipment, is inexpensive, and can be performed by most competent dentists. It does, however, need considerab[ le accuracy and a thorough understanding of the mucocele and its surrounding anatomy.7 In our case report, we used a scalpel to remove the lesion. We didn't have a lot of bleeding, and the healing process went smoothly. We chose this procedure because it is less invasive and less expensive than laser ablation, cryosurgery, and electro cautery. But the recurrence was seen as the underlying gland was resected completely at first and also there was mechanical trauma caused by the upper lateral incisor. Oral Mucoceles recurred more frequently, with a statistically significant difference, in younger patients (aged 30 years,16.0%) than in older patients, according to the research (aged 30 years, 4.4%).10
Marsupialization has resulted in considerably higher recurrence rates. Micro marsupialization has been believed to have reduced recurrence rates since histological inspection is not available. However, it is restricted to lesions with clinical features that strongly support a mucocele diagnosis.11
Cryosurgery had positive outcomes with no recurrences. However, considerable oedema and discomfort were noted as postoperative effects, as well as a protracted healing time.12
Vaporization using argon and Nd: YAG lasers has been described as a novel way of treating mucoceles. Both laser treatments yielded good outcomes with minimal recurrence rates and were well tolerated by patients, the major complaint of whom being pain.13 The most significant advantages of soft tissue laser applications are reduced intraoperative bleeding, edoema, and postoperative discomfort., as well as very little surgical time, scarring, and coagulation, with no need for suturing after excision due to natural wound dressing caused by denatured proteins.9
Conclusion
Mucoceles are one of the most common oral cavity soft tissue lesions causing patient discomfort and distress. Of the numerous advanced methods of treatment, simple surgical excision is a choice treatment that can alleviate patient fear and anxiety. Managing mucocele is a difficult task due to high opportunities for recurrence. However, with least recurrence, surgical excisions were successful when dissected from the surroundings and contributing small saliva gland acini.